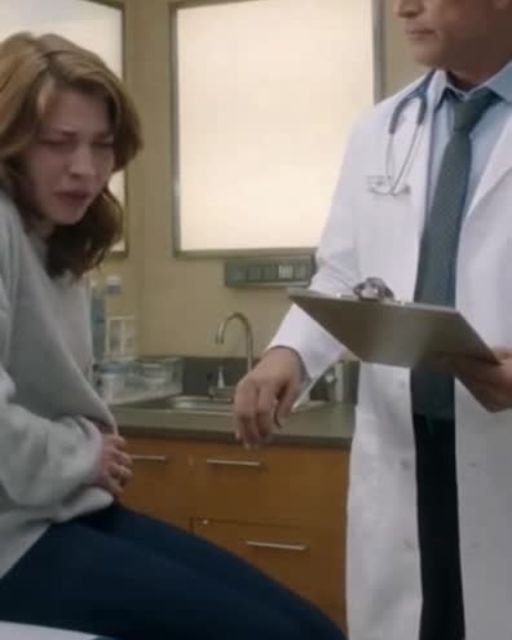
“It’s probably anxiety,” he said without even looking up from the chart. I sat there, clutching the paper gown around me, trying not to cry from the frustration—not the pain.
I’d been short of breath for months. Tight chest, dizzy spells, waking up in the middle of the night gasping.
I knew something was wrong. But he barely asked me three questions before waving it off.
“Try some deep breathing. Maybe cut back on caffeine,” he said with a shrug. I left that appointment humiliated… and still struggling to breathe.
Two weeks later, I nearly passed out at work and ended up in urgent care. Different doctor. Different tone.
She ordered a chest scan immediately. She called it “just to be safe,” but I saw the look in her eyes.
Then came the techs, the whispers, the extra images. And finally, the words I’ll never forget: “There’s a mass pressing against your lung.”
Benign, thank God. But big. Too big to ignore.
It had been growing for months. That first doctor—the one who told me to “relax”? Let’s just say he got a copy of the scan delivered straight to his office with my name on it.
I didn’t expect anything dramatic to happen after the scan was sent. I honestly thought he’d ignore it or pretend he’d never seen me.
But the fallout came quicker than I imagined. Three days after my surgery consult, I got a voicemail from the clinic manager asking me to “come in to discuss my previous visit.”
Her voice sounded stiff and rehearsed, like someone was listening to make sure she said everything correctly. I almost deleted it.
I didn’t want to go back there. I didn’t want to sit in that same room where I’d felt small, dismissed, and stupid for daring to say something didn’t feel right.
But my sister insisted I go. She said people like him get away with things because people like me don’t follow up.
So I went. I walked into that clinic with my chest still aching and my breathing uneven.
The first person I saw was the nurse from my earlier appointment. Her name tag read Mara, and she looked different this time—less rushed, more serious.
She pulled me aside before I even reached the waiting room. “I’m really glad you came,” she said softly.
“You shouldn’t have been treated the way you were.” I felt tears rush up again, but this time from being seen.
“I don’t know if they told you why you’re here,” she continued, “but you should hear the truth from me, not from a meeting script.” My stomach tightened.
She lowered her voice and leaned closer. “You weren’t the first.”
That sentence hit me harder than the diagnosis. A part of me had hoped my case was just a fluke—a missed detail, a bad day, something forgivable.
But the way she said it—with anger and exhaustion mixed together—told me everything I needed to know. She guided me to a small side room and closed the door.
“Look,” she said, rubbing her forehead, “I’ve worked with him for almost two years.” Every time a woman comes in with pain he can’t see immediately, he labels it as stress or anxiety.
“Unless she’s over sixty, then he checks for heart issues. Anyone younger? He says it’s ‘in their head.’”
My hands were shaking, not from fear but disbelief. “And you tried to report it?” I asked.
“Twice,” she said. “Once to the clinic manager and once to HR.”
“They told me to focus on workflow and stop questioning the physicians.” I let out a bitter laugh.
“Of course.” She met my eyes. “But your scan? That changed everything.”
Apparently, when he received the copy of my scan, he panicked. Not out of concern for me, but because there was proof he’d dismissed me without proper evaluation.
He rushed to update my chart, adding notes that weren’t there before. He even tried to change the timestamp on one of the entries.
But the system logs everything. Mara saw the edits.
She printed the logs and the original chart. Then she sent them both anonymously to the clinic manager.
That’s when things spiraled. The manager called him in for a meeting.
Instead of owning up, he blamed everyone else. He said the equipment was slow that day and claimed the nurse didn’t give him the full history.
He even said I “seemed fine and didn’t express concern.” When they asked why he never ordered even a basic lung check, he said, “She looked anxious.”
The manager didn’t tell me all this directly. Mara did, because she thought I deserved to know.
But the real twist came next. “There’s something else,” she said.
“Another patient filed a complaint last year. Very similar to yours.”
Shortness of breath, fatigue, chest tightness. He told her it was anxiety too.
“She ended up in the ER with a collapsed lung two months later,” Mara said. My whole body went cold.
“Is she okay?” I asked. “She recovered,” Mara replied. “But she never came back here.”
She paused and added, “A lot of women never come back.” I felt a wave of rage and heartbreak crash over me.
Rage that he was allowed to keep practicing. Heartbreak for every woman who left that clinic doubting her own instincts.
What cut deepest was knowing how close I came to being another silent case. The clinic manager eventually joined us in the room.
Her tone had that same careful professionalism from the voicemail, but there was unease under it. “Thank you for meeting with us,” she began.
“We’re conducting a formal review of your previous appointment. We want to ensure all patients feel heard and safe.”
It sounded like something she’d practiced in a mirror. A part of me wanted to shout at her for not listening to Mara sooner.
Instead, I asked, “So what are you doing about him?” She hesitated.
“He’s been placed under internal investigation,” she said. I raised an eyebrow. “Meaning what? He’s still seeing patients?”
“For the moment, yes,” she answered, shifting her gaze. That reply punched the air out of my lungs.
I stood up. “Then why am I here?”
“We wanted to gather your perspective,” she replied. “No,” I said. “You want to cover yourselves.”
“You want to say you addressed patient concerns without actually protecting patients.” Mara looked at me with pride, like she’d been waiting for someone to say it.
The manager straightened. “We are following protocol.” I shook my head. “Your protocol is why this keeps happening.”
I walked out before she could respond. Mara followed me to the exit.
“I’m sorry,” she said quietly. “I wish they took action sooner.”
I squeezed her hand. “You tried. That matters. And now that I know, I’m not staying quiet.”
She nodded with relief. “Good. That’s what it’ll take.”
I didn’t plan on doing anything dramatic. I wasn’t aiming for revenge.
But I did want accountability. So I wrote everything down—every symptom, every detail, every dismissive comment.
I attached copies of the scan reports, urgent care notes, and the surgeon’s recommendation. Then I sent the whole packet to the state medical board.
I didn’t expect a quick response. Those things usually take months.
But three weeks later, I received a letter saying they were opening a formal investigation. Then something unexpected happened.
The woman who’d had the collapsed lung—the one Mara told me about—reached out to me. With my permission, Mara had given her my email.
Her name was Rina. She told me she had tried to file a complaint before, but without supporting cases, her claim went nowhere.
Now she had one. Then another woman emailed. Then a third.
All with similar stories. All dismissed. All told they were anxious.
Most had ended up in emergency rooms. That’s when I realized this wasn’t just about me.
This was a pattern—a dangerous one. So I helped them organize their reports.
We submitted them together, each documenting our separate experiences. We connected them through the same doctor, the same dismissals, the same consequences.
That’s when the momentum shifted. Two months later, the doctor resigned quietly.
But the story didn’t end there. A local journalist reached out.
Someone inside the clinic had leaked the situation. Someone wanted the truth out.
The reporter didn’t use our names without permission, but she described the pattern clearly. People recognized the clinic and the issue.
The article caused a storm—not of pitchforks, but of voices saying, “This happens too often. Enough is enough.” Comments poured in.
Women shared almost identical experiences. Not always with him, but with other doctors who dismissed their pain, their instincts, their bodies.
The article went viral in our area. Then came a twist I never saw coming.
The clinic manager contacted me again—but not to defend him. She apologized.
This time it wasn’t stiff or scripted. It sounded real.
The medical board’s investigation uncovered a long trail of altered charts, ignored symptoms, and complaints that never became official records. Someone higher up had been burying them.
That person was fired. The manager told me changes were already being made.
Mandatory symptom protocols, outside audits, anonymous nurse reporting, and a patient advocacy program were being introduced. They even asked if I’d speak to their staff about my experience.
I thought about saying no. Then I remembered myself sitting in that paper gown, barely able to breathe, fighting to be heard.
So I said yes. The room was full of doctors, nurses, assistants, and admin staff.
My chest tightened as I spoke, not from fear but from remembering everything. When I finished, people looked genuinely moved.
Some apologized personally. And Mara hugged me so tightly I almost cried again.
“You did it,” she whispered. “You finally made them listen.” The biggest twist came months later.
At a follow-up, my surgeon told me the mass had probably been there for over a year. Slowly growing, slowly pressing, slowly suffocating me.
If I hadn’t pushed for answers—and if the urgent care doctor hadn’t taken me seriously—I could’ve lost more than my breath. I could’ve lost my life.
The weight of that truth hit me in waves over time. But so did something else: gratitude.
Not the cheesy kind, but the kind that comes from realizing even the worst moments led to something that mattered. The doctor who dismissed me never returned to practice.
The clinic improved its systems. Women who once doubted themselves began trusting their instincts again.
And Mara—brave, persistent, underappreciated Mara—was promoted to a supervisory role where her reports couldn’t be buried. As for me, I healed.
The surgery went well, and my breathing grew easier week by week. The emotional healing took longer.
Some nights I still woke up wondering if I was imagining symptoms again. Then I’d place my hand on my chest, feel the steady rise and fall, and remember that my voice saved me.
It saved others too. The lesson is simple but hard-earned: trust your instincts.
If something feels wrong, don’t let anyone—doctor or not—tell you it’s all in your head. Your body speaks.
You just have to listen. And if someone refuses to hear you, find someone who will.
Your health, your safety, your life—they’re worth fighting for. And sometimes, speaking up helps more people than you realize.
If this story moved you or reminded you of someone who needs to hear it, please share it and give it a like. Someone out there might need the reminder that their voice matters.